Imagine a silent, widespread passenger within the human population, the Merkel cell polyomavirus (MCPyV). Most of us harbor this virus, our immune systems likely having encountered and kept it in check without us ever knowing. Yet, in a tiny fraction of individuals, this seemingly innocuous virus becomes entangled in the development of a rare and aggressive skin cancer: Merkel cell carcinoma (MCC). This perplexing situation is what researchers have dubbed the “Merkel Cell Carcinoma Virus Conundrum,” a multifaceted puzzle that continues to intrigue and challenge the scientific community.
At the heart of this conundrum lie several key paradoxes:
Ubiquity vs. Rarity: A Common Virus, an Uncommon Cancer: The sheer prevalence of MCPyV is striking. Antibodies against it are found in a significant portion of the adult population, indicating widespread exposure. This starkly contrasts with the rarity of MCC. Why does a virus so common trigger cancer in so few? What other factors are at play that tip the balance from benign coexistence to malignant transformation?
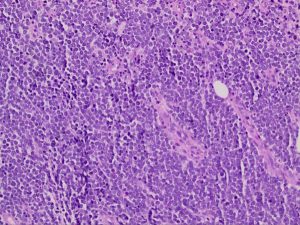

The Enigmatic Mechanism of Oncogenesis: In a majority of MCC cases (around 80%), the DNA of MCPyV is found integrated directly into the tumor cells. This strong association suggests a causal link. The virus produces proteins called T antigens, some of which are believed to interfere with crucial tumor suppressor proteins within the cell. However, the precise molecular choreography by which MCPyV hijacks cellular machinery and drives uncontrolled growth remains an active area of investigation. The full script of viral oncogenesis is still being written.
The Virus-Negative Enigma: Adding another layer of complexity, approximately 20% of MCC cases show no detectable signs of MCPyV. This crucial observation reveals that other pathways, most notably those driven by mutations caused by ultraviolet (UV) radiation, can independently lead to this cancer. Comparing and contrasting virus-positive and virus-negative MCC is a vital avenue of research, as these two subtypes can exhibit distinct genetic profiles and clinical behaviors, potentially requiring different therapeutic approaches.
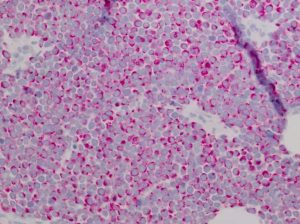
The Immune System’s Double-Edged Sword: The role of the immune system in the MCC story is undeniable. Individuals with compromised immunity, such as transplant recipients or those with HIV, face a dramatically elevated risk of developing MCC. This underscores the immune system’s usual effectiveness in controlling MCPyV and preventing virus-driven cancer. Intriguingly, in patients with virus-positive MCC, a robust immune response against the virus within the tumor is often associated with better treatment outcomes. This highlights the delicate balance between viral presence and the host’s ability to fight back.
Causality Under Scrutiny: While the consistent presence of MCPyV in most MCC tumors strongly suggests a causal role, definitively proving it according to traditional Koch’s postulates for infectious diseases presents a unique challenge due to the virus’s widespread nature and the cancer’s rarity. Instead, researchers rely on a wealth of molecular evidence, such as the consistent integration of the viral genome at specific sites within tumor DNA, to build a compelling case for viral causality in a significant proportion of MCC cases.
The Cell of Origin: A Lingering Mystery: Even the very cell from which MCC arises remains a subject of debate. Despite the name implicating Merkel cells (specialized touch receptor cells in the skin), these cells are terminally differentiated and not thought to undergo cell division. Current research points towards a potential precursor cell or even, surprisingly, a B-cell lineage in some instances. This uncertainty further complicates our understanding of how MCPyV might initiate the transformation process.
Why Unraveling the Conundrum Matters:
Deciphering the intricacies of the Merkel cell carcinoma virus conundrum is not merely an academic exercise. It holds significant promise for tangible improvements in patient care:
- Sharpening Risk Assessment: Identifying the specific co-factors or host characteristics that predispose MCPyV-infected individuals to develop MCC could allow for more precise risk stratification and potentially earlier intervention.
_______________________________ - Paving the Way for Early Detection: A deeper understanding of the initial stages of virus-driven tumor development could lead to the creation of novel diagnostic tools for earlier detection, when treatment is often most effective.
_______________________________ - Tailoring Treatment Strategies: Recognizing the differences between virus-positive and virus-negative MCC, and appreciating the critical interplay between the virus and the immune system, could enable the development of more personalized and effective treatment approaches. The success of immunotherapies in treating MCC, regardless of viral status, underscores the importance of harnessing the body’s own defenses.
_______________________________ - Exploring Prevention Strategies: While preventing infection with a ubiquitous virus like MCPyV is likely impractical, identifying co-factors such as excessive UV exposure or specific immunosuppressive conditions that might elevate the risk of MCC in infected individuals could lead to targeted preventative measures.
_______________________________
In conclusion, the “Merkel Cell Carcinoma Virus Conundrum” encapsulates a fascinating and complex interplay between a common, often silent virus and a rare, aggressive cancer. While we are humbled with the fact that there is a lot we don’t know about this virus, the ongoing quest to unravel the mysteries surrounding this association promises to yield crucial insights into the fundamental mechanisms of cancer development, ultimately leading to improved risk assessment, earlier diagnosis, and more effective treatment strategies for this challenging disease. The intricate dance between virus, host, and environment continues to be a central focus of dedicated scientific inquiry.